Type 2 Diabetes Management
The Sugar Shakedown
Ever felt like your blood sugar levels are a rollercoaster you can't get off? You're not alone. Managing Type 2 Diabetes can be a daily struggle, leaving you feeling frustrated and anxious about your health. But what if there was a way to break free from these struggles and reclaim your health and happiness?
The Sugar Shakedown is our program designed to help you take control of your diabetes, naturally. With personalised physical activity and nutrition plans, we show you how to focus on controlling blood sugar levels and achieving a healthier body weight, attitude, and outlook on life. Our approach isn't about strict diets or intense workouts - it's about finding what works for you and making sustainable lifestyle changes.
Imagine waking up each morning feeling energised and excited about the day ahead. Picture yourself enjoying delicious, natural foods that nourish your body and soul. With The Sugar Shakedown, you'll feel great physically, mentally and emotionally. Say goodbye to the stress and anxiety of managing diabetes, and hello to a life filled with vitality, confidence, and joy. You'll not only improve your health and manage your diabetes, but you'll also rediscover the joy of movement and the pleasure of eating well. It's time to take back control of your health and start living life on your own terms.
What is Type 2 Diabetes?
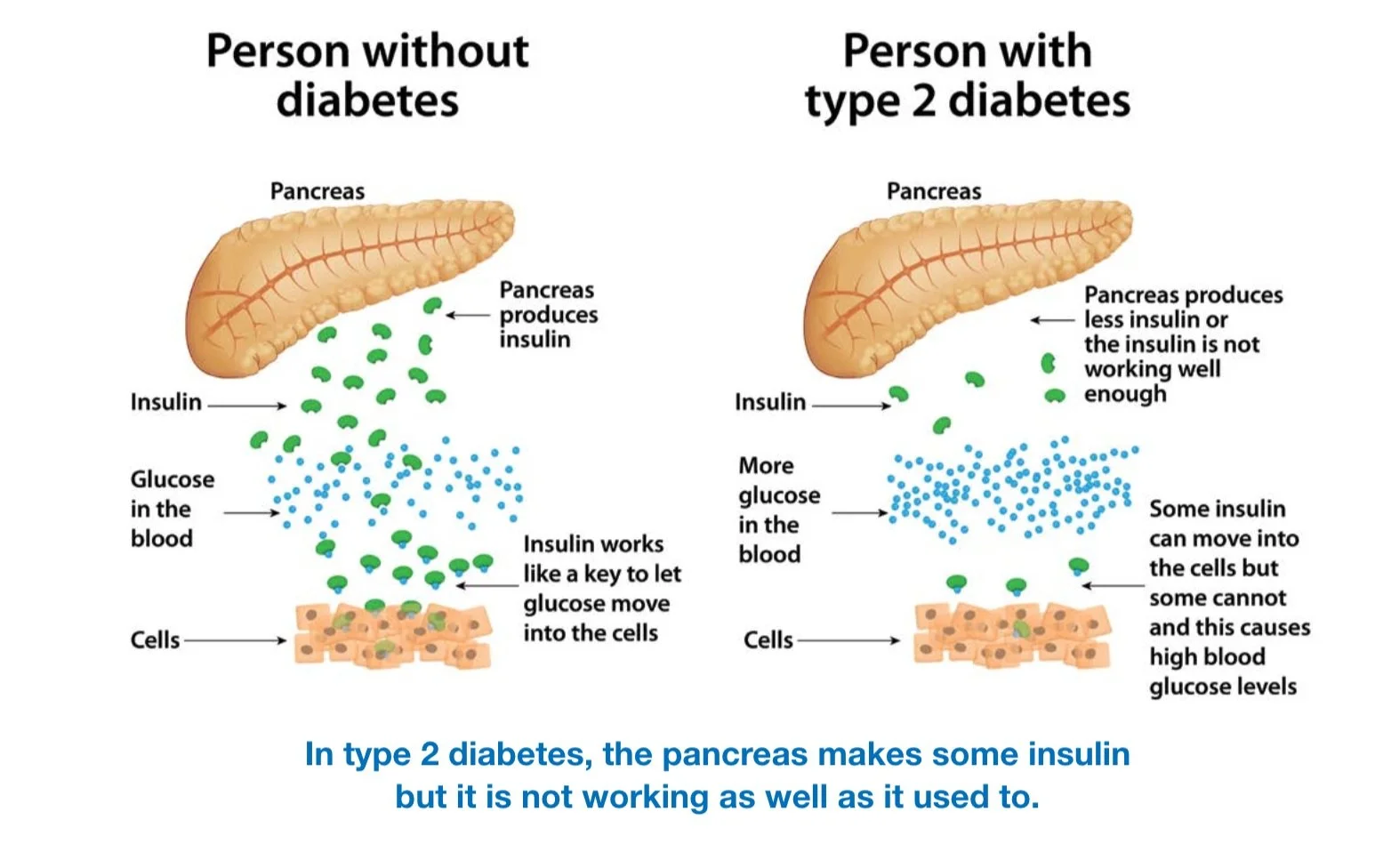
Type 2 Diabetes is a chronic condition that affects how your body metabolises sugar (glucose), which is your body's main source of energy. In Type 2 Diabetes, your body either resists the effects of insulin (a hormone that regulates the movement of sugar into your cells) or doesn't produce enough insulin to maintain normal glucose levels.
This results in high levels of sugar building up in your bloodstream, which can lead to a variety of serious health complications if not properly managed. Type 2 Diabetes is often associated with lifestyle factors such as obesity, lack of physical activity, and poor diet, although genetics and family history also play a role.
Symptoms of Type 2 Diabetes can include increased thirst, frequent urination, unexplained weight loss, fatigue, blurred vision, and slow-healing sores or infections. However, some people with Type 2 Diabetes may not experience any symptoms initially.
Managing Type 2 Diabetes involves making lifestyle changes such as adopting a healthy diet, increasing physical activity, monitoring blood sugar levels, and taking medications or insulin. With proper management, many people with Type 2 Diabetes can live healthy, active lives and reduce their risk of complications.
How Can We Help You Manage Type 2 Diabetes?
Dietetics for Type 2 Diabetes
Our dietitians help people with Type 2 Diabetes adopt a healthy diet that promotes better blood sugar control, weight management, and overall well-being for long-term success.
Personalised Nutrition Plans: Our dietitians work closely with each person to develop a personalised nutrition plan tailored to their unique needs, preferences, and lifestyle. This plan takes into account factors such as medical history, current health status, dietary preferences, cultural considerations, and any other relevant factors.
Blood Sugar Management: Our dietitians educate people about how different foods affect blood sugar levels and provide practical strategies for managing blood sugar through diet. This may include guidance on carbohydrate counting, portion control, choosing foods with a low glycemic index, and timing meals and snacks appropriately.
Balanced Nutrition: Our dietitians emphasise the importance of a balanced diet that includes a variety of nutrient-rich foods from all food groups. We provide guidance on incorporating plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats into daily meals and snacks to ensure adequate nutrition while managing blood sugar levels.
Healthy Eating Habits: Our dietitians help people develop healthy eating habits that support long-term success. This may include mindful eating practices, such as paying attention to hunger and fullness cues, practising portion control, and avoiding emotional eating or eating out of boredom.
Meal Planning and Preparation: Our dietitians assist people with meal planning and preparation to make healthy eating easier and more convenient. We provide practical tips for grocery shopping, meal prepping, cooking healthy meals at home, and making healthier choices when dining out or on the go.
Education and Empowerment: Our dietitians empower people with the knowledge and skills they need to make informed decisions about their diet and lifestyle. We provide education about nutrition, diabetes management, label reading, and other relevant topics to help people take control of their health and make positive changes.
Ongoing Support and Accountability: Our dietitians provide ongoing support and accountability to help people stay motivated and on track with their dietary goals. We are available to answer questions, address concerns, provide encouragement, and make adjustments to the nutrition plan as needed.
Exercise Physiology for Type 2 Diabetes
Our exercise physiologists help people with Type 2 Diabetes increase their physical activity levels in a safe and effective manner.
Individualised Exercise Prescription: Our exercise physiologists conduct a thorough assessment of each individual's current fitness level, medical history, and any specific needs or limitations. Based on this assessment, we develop a personalised exercise prescription tailored to the person’s goals, abilities, and preferences.
Education about Exercise and Diabetes: Our exercise physiologists provide education about the benefits of exercise for managing Type 2 Diabetes, including improved blood sugar control, weight management, cardiovascular health, and overall well-being. We also educate people about how different types of exercise affect blood sugar levels and provide guidance on safe and effective exercise practices.
Exercise Programming: Our exercise physiologists design a structured exercise program that includes a variety of aerobic, strength training, and flexibility exercises. We provide guidance on the frequency, intensity, duration, and progression of exercises to help people achieve their goals while minimising the risk of injury or complications.
Monitoring and Progress Tracking: Our exercise physiologists monitor people’s progress throughout their exercise program and make adjustments as needed to ensure continued improvement. We track key indicators such as fitness levels, blood sugar levels, weight, and other relevant metrics to assess progress and make informed decisions about the exercise prescription.
Motivation and Support: Our exercise physiologists provide motivation, encouragement, and support to help people stay motivated and adhere to their exercise program. We offer guidance on overcoming barriers to exercise, setting realistic goals, and maintaining a positive mindset throughout the journey.
Integration with Lifestyle and Preferences: Our exercise physiologists take into account each person’s lifestyle, preferences, and personal interests when designing their exercise program. We help people find activities they enjoy and can incorporate into their daily routine, whether it's walking, swimming, cycling, strength training, yoga, or any other form of physical activity.
Collaboration with the Larger Healthcare Team: Our exercise physiologists work collaboratively with people’s larger healthcare team, including their GP, diabetes educator, dietitian, and other healthcare professionals, to ensure coordinated care and optimal management of Type 2 Diabetes.
Diabetes Education
Our diabetes educator helps people with Type 2 Diabetes effectively manage their condition and improve their overall health and well-being.
Diabetes Self-Management Education: Our diabetes educator provides comprehensive education about Type 2 Diabetes, including its causes, symptoms, complications, and treatment options. He helps people understand the importance of blood sugar monitoring, medication management, healthy eating, physical activity, and other aspects of diabetes self-care.
Medication Management: Our diabetes educator provides education and support regarding medication management for Type 2 Diabetes. He helps people understand the purpose, dosage, administration, and potential side effects of their medications, as well as strategies for adhering to their prescribed medication regimen.
Blood Glucose Monitoring: Our diabetes educator teaches people how to monitor their blood glucose levels effectively using glucometers or continuous glucose monitoring devices. He provides guidance on when and how often to test blood sugar, how to interpret blood glucose readings, and what actions to take based on the results.
Nutrition Counseling: Our diabetes educator provides individualised nutrition counseling to help individuals with Type 2 Diabetes make healthy food choices that support blood sugar control, weight management, and improved overall health. He will offer guidance on meal planning, carbohydrate counting, portion control, label reading, and making healthier food choices when dining out or grocery shopping.
Lifestyle Modification: Our diabetes educator supports individuals in making lifestyle modifications to improve their overall health and wellbeing. This may include smoking cessation, stress management, sleep hygiene, and other lifestyle factors that can impact diabetes management and overall health.
Psychosocial Support: Our diabetes educator offers psychosocial support to people with Type 2 Diabetes to address emotional and psychological aspects of living with a chronic condition. He provides counseling, coping strategies, and resources to help people navigate the emotional challenges associated with diabetes and maintain a positive outlook on life.
Continuous Monitoring and Support: Our diabetes educator provides ongoing monitoring and support to people with Type 2 Diabetes to ensure they are effectively managing their condition and making progress towards their health goals. He is available to answer questions, address concerns, provide encouragement, and make adjustments to the diabetes management plan as needed.
Your GP will be the best person to discuss the right medication or insulin.
Why Choose The Allied Health Team to Help You Manage Type 2 Diabetes?
People with Type 2 Diabetes stand to gain immense benefits from engaging with our comprehensive support system. With a team of experienced dietitians, exercise physiologists, and a dedicated diabetes educator, we offer tailored solutions to address every aspect of diabetes management. Our dietitians provide personalised nutrition plans to help individuals achieve better blood sugar control and weight management, while our exercise physiologists design safe and effective exercise programs to increase physical activity levels and improve overall health. Additionally, our diabetes educator offers valuable education, support, and guidance to empower individuals to understand and manage their condition effectively. By combining expertise in diet, exercise, and diabetes education, we provide holistic care that enables individuals to lead healthier, more fulfilling lives with Type 2 Diabetes.
For more information about Type 2 Diabetes, check out the National Diabetes Services Scheme website, put together by Diabetes Australia: https://www.ndss.com.au